Vitamin D
October 15, 2020
Vitamin D (cholecalciferol) is a nutrient found in some foods like fatty fish that can be added to your diet as a supplement. Our body makes vitamin D when our skin is directly exposed to the sun, and most people meet at least some of their vitamin D needs this way. Vitamin D is required to maintain healthy bones, carry messages between the brain and the body, and fight off infections.
An estimated 1 billion people worldwide are vitamin D deficient or insufficient. And it seems that vitamin D levels are decreasing with time. The reasons for this deficiency are many (pollution, increased use of sunscreen, etc.); however, increased time spent indoors and obesity are likely to play a central role.
Currently, we see more publications on the possible relationship between vitamin D levels and COVID-19 severity. Recent research suggests that vitamin D deficiency may increase the risk of coronavirus infection and severity of COVID-19. Most of these studies are observational studies, and clinical trials are needed to verify these initial findings.
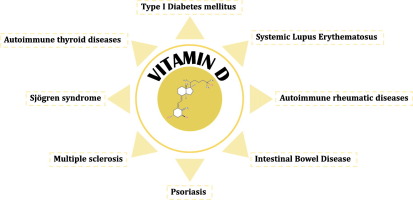
Vitamin D deficiency is also associated with autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, type 1 diabetes mellitus, and multiple sclerosis. The prevalence of vitamin D deficiencies in autoimmune disease patients is high, and vitamin D supplementation is considered beneficial, lessening disease severity.
Five to eight percent of the world’s population is currently affected by 80 to 100 autoimmune diseases. The incidence has been steadily increasing in recent years, reaching alarmingly high numbers, particularly for type 1 diabetes mellitus, Crohn’s disease, rheumatoid arthritis, Sjogren’s syndrome, and multiple sclerosis.
Current treatment approaches are primarily symptomatic or suppress the immune system. However, recent studies reveal significant benefits of nutrition-related therapeutic approaches, including prevention and the treatment of established disease, which offer a cost-efficient and trigger-unspecific alternative of balancing rather than suppressing the immune system. Vitamin D and zinc are currently the best-studied and most promising candidates for therapeutic intervention.
Although no papers were found on the possible role of vitamin D in AE, there are publications exploring vitamin D’s role in neuromyelitis optica spectrum disorder (NMOSD) that could be indicative of AE. NMOSD is an autoantibody-mediated disease affecting the central nervous system. Evidence suggests that low vitamin D levels may associate with disease activity and relapse rate in NMOSD, indicating the participation in the pathogenesis of NMOSD.
More on Vitamin D
After its uptake, vitamin D is converted into 25(OH)D and then into the biologically active metabolite 1,25(OH)2D (calcitriol) in the liver and kidneys, respectively. Evidence suggests that Vitamin D plays a vital role in influencing T-cell and B-cell responses and disrupting the production of cytokines. Some of the demonstrated immunomodulatory effects are:
- a reduction in the production of interleukin-2 (IL-2), gamma interferon (INF-γ), and tumor necrosis factor (TNF);
- inhibition of the expression of IL-6;
- inhibition of the secretion and production of autoantibodies by B lymphocytes.