Our Research Efforts
International Consensus Recommendations for the treatment of pediatric NMDAR Antibody Encephalitis.
DR. NOSADINI AND DR. DALE, 2021
The paper results from the hard work, dedication, and collaboration between 27 international AE experts, led by Dr. Margherita Nosadini and Dr. Russell Dale. These treatment recommendations will be of great value to children affected by AE and clinicians worldwide.
The recommendations start with general management principles, highlighting the importance of early diagnosis and careful communication with the family. The importance of raising awareness of this disorder, which may first present to psychiatrists and emergency physicians as well as neurologists, cannot be overemphasized, and the diagnostic criteria (2016) and modification for children (2020), along with the distinctive clinical characteristics, may help to get to a speedy diagnosis. Families need to be informed of the expected or potential disease evolution, the treatment possibilities, and the often long and demanding course of the illness.
Highlights of the Consensus-based Recommendations of the treatment of Pediatric NMDAR antibody encephalitis:
– Corticosteroids are recommended in all children with NMDARE, with additional IV immunoglobulin or plasma exchange in severe patients.
– Prolonged first-line immunotherapy can be offered for up to 3–12 months (oral corticosteroids or monthly IV corticosteroids/immunoglobulin), dependent on disease severity.
– Second-line treatments are recommended for cases refractory to first-line therapies (rituximab preferred over cyclophosphamide) and should be considered about two weeks after the first-line initiation.
– Further immunotherapies for refractory disease 1-3 months after second-line initiation include another second-line treatment (such as cyclophosphamide) and escalation to tocilizumab.
– Maintenance immune suppression beyond six months (such as rituximab redosing or mycophenolate mofetil) is generally not required, except for patients with a more severe course or prolonged impairments and hospitalization.
– For patients with relapsing disease, second-line and prolonged maintenance therapy should be considered.
– The treatment of NMDARE following herpes simplex encephalitis should be similar to idiopathic NMDARE.
– Broad guidance is provided for the total treatment duration (first line, second line, and maintenance), dictated by the severity and clinical course (i.e., median 3, 9, and 18 months in the best, average, and worst responders, respectively).
– Although tumors are rare in prepubertal children and boys, oncologic searches for ovarian teratoma (and neural crest tumors in children aged <5 years) are mandatory in all children with NMDARE, and should be performed early and completed in the first days-weeks after admission.
AE Alliance would like to thank Dr. Nosadini and Dr. Dale, and all the physicians involved, that have worked tirelessly to make these treatment recommendations for NMDARE possible. We would also like to thank the De Vivero Family for their support and input.
Read the full article here.
Autoimmune encephalitis: proposed best practice recommendations for diagnosis, acute-, symptomatic-, and long-term management.
DR. HESHAM ABBOUD, UNIVERSITY HOSPITALS OF CLEVELAND, CASE WESTERN RESERVE UNIVERSITY, CLEVELAND, OHIO, 2021
We are excited to report the first international best practice recommendations for the management of autoimmune encephalitis. The papers result from the hard work and collaboration between 68 AEA Clinicians Network members from 17 countries, initiated and led by Dr. Hesham Abboud. These recommendations will be of great value to AE patients and clinicians all over the world.
AE is possibly as common as infectious encephalitis, and the rapidly advancing knowledge of new antibodies and their associated syndromes has created a new and growing field of autoimmune neurology. However, these advances have not been paralleled by advancement in clinical practice, leading to a large knowledge gap regarding the acute and long-term management of AE. Currently, the results of antibody testing panels are not available at early evaluation and management of AE, so physicians have to approach AE initially as a clinical entity when deciding on tests and treatments. Long-term management can then be modified according to the type of antibody identified.
These papers aim to evaluate available evidence for each step in the management of AE as a broad category, and to provide an expert opinion when evidence is lacking to come to best practice recommendations for management of AE. What makes these recommendations stand out is that these represent the practice of experienced clinicians from different clinical and geographical backgrounds.
In this first part of the best practice recommendations, Dr. Abboud and colleagues cover the diagnosis and acute management of AE guided by published studies and the results of the AEACN survey providing updated guidance for the management of patients with suspected AE. The second part focuses on bridging therapy, symptomatic treatment and maintenance immunotherapy.
Clinical approach to the diagnosis of autoimmune encephalitis in the pediatric patient
TANIA CELLUCI, McMASTER CHILDREN’S HOSPITAL, CANADA, 2020
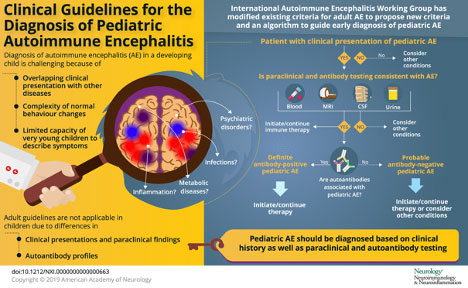
Autoimmune encephalitis (AE) is an important and treatable cause of acute encephalitis. Diagnosis of AE in a developing child is challenging because of overlap in clinical presentations with other diseases and the complexity of normal behavior changes. Existing diagnostic criteria for adult AE require modification to be applied to children, who differ from adults in their clinical presentations, paraclinical findings, autoantibody profiles, treatment response, and long-term outcomes.
At the 2014 Autoimmune Encephalitis Alliance conference in North Carolina, the Autoimmune Encephalitis International Working Group was formed and initiated discussions around developing diagnostic criteria for AE. A subcommittee of pediatric neurologists and rheumatologists identified that adult-focused criteria may not apply well to children. As a result, this subcommittee collaborated through conference calls and email correspondence to consider the pediatric-specific approach to AE. Click here for the full article
Clinical Trial of IVIG in LGI1/CASPR2 Encephalitis
DR. SEAN PITTOCK, MAYO CLINIC CENTER FOR MULITPLE SCLEROSIS AND AUTOIMMUNE NEUROLOGY, MN, 2020
This first randomized, double-blind placebo-controlled trial evaluated the efficacy of IVIG in reducing seizure frequency in LGI1 and CASPR2 encephalitis patients. The doctors contacted 594 patients, of which only 17 met the criteria and were entered into the study.
Despite challenges and limitations, 75% of patients (all LGI1), in the IVIG group experienced more than a 50% reduction in seizure frequency (some patients had more than 60 seizures per day at the start of the trial), compared to 22% in the placebo group. A trend towards more positive cognitive outcomes (stable and improved thinking) was observed in the IVIG group, compared to the placebo group, although there was no statistical difference. Of the IVIG group, 25% achieved seizure freedom by the end of the trial.
This study is especially important for patients in whom corticosteroids are contraindicated or for those not responding to corticosteroid therapy. The data supports the consideration of IVIG as a therapeutic option in these cases and may be supportive in obtaining insurance approval for IVIG. Click here for the full article.
Understanding Consequences of Encephalitis
DR. ARUN VENKATESAN OF THE JOHNS HOPKINS UNIVERSITY IN BALTIMORE & DR. ANUSHA YEKOSHUMAR OF THE ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI HOSPITAL IN NEW YORK CITY. 2019
While encephalitis may result in the development of a number of persistent symptoms, these have not been well studied. A better understanding of the persistent symptoms in people affected by encephalitis may lead to the development of targeted therapeutic and rehabilitation measures to enhance function and quality of life.
This study will include patients between 18 – 84 years of age who are diagnosed with any form of encephalitis. Participants will be recruited from the Autoimmune Encephalitis Alliance, Encephalitis Society and several clinics.
Changes in Language Throughout Symptom Onset and Recovery in Individuals with Anti-NMDA Receptor Encephalitis
DR. ANUSHA YEKOSHUMAR AND KELSEY E MARTIN OF THE ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI HOSPITAL IN NEW YORK CITY. 2019
Anti-NMDA receptor encephalitis (anti-NMDARE) is a form of autoimmune encephalitis typically characterized by early psychiatric symptoms that progress to seizures, abnormal movements, and alterations in consciousness. Few studies have explored early cognitive changes, such as language, or psychiatric prodromal symptoms of the disease. This study will focus on analysis of early changes in language, supported by studies demonstrating that changes in coherence and complexity predict onset of first break psychosis.
Long-term outcomes study in autoimmune encephalitis
DR. ANUSHA YEKOSHUMAR OF THE ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI HOSPITAL IN NEW YORK CITY. 2018
The Autoimmune Encephalitis Alliance is participating in a study to better understand the challenges AE survivors face during recovery and in the years following diagnosis. There is a survey designed for caregivers as well, which will provide useful information to researchers. We hear from many patients who are facing ongoing struggles to return to life as “normal” and caregivers desiring to help their loved ones recover. We hope this study will shed new light on the needs in this area and lead to advances in rehabilitation that will ultimately benefit patients and caregivers. Click here to read the article.