My brother’s AE journey
Steve! It’s Mom. I don’t know what’s going on. Joseph woke up having seizures this morning. He’s at the hospital. I’m on my way there now. Call me!” I would listen to this harrowing voicemail about an hour after it was received. Mom was right. Suddenly, Joe was having seizures when he’d never had them before. Within those first couple hours, the hospital hadn’t been able to get the seizures under control and nobody had any indication how this could be happening. It was early November, yet while leaving the house that morning to go to the hospital, it felt like the darkness of winter had come early for 2017.
Mom’s voicemail was my first indicator that something was going on. I’d come to learn that Joe hadn’t been feeling well for a bit now. It seemed like common flu; he was lethargic and had a mild fever. After about five days, these symptoms hadn’t subsided and he started to exhibit other signs that something wasn’t right. A couple of emergency room visits resulted in a few scans and blood work that provided no more relative information about what’s causing his symptoms, which had gotten worse. What looked like common flu turned to delirium, urinary retention, and ptosis. Yet, Joe was discharged. When he left the ER and returned home, nobody had any idea that, in a day, Joe would be back in the hospital after having his first seizure and wouldn’t see the outside again for a long, long time.
When I arrived at the hospital that first morning, it was already evident that Joe was now in a fight for his life. We could see the seizures were more frequent. The seizures were accompanied by heavy tremors that we’d later learn to be myoclonic jerks. These jerks presented throughout his limbs which left Joe in a state of perpetual trembling and complete unconsciousness. In addition to the visible shaking, his autonomic nervous system (ANS) had flown into complete chaos. This was causing extremely dangerous fluctuations in heart rate and blood pressure while also putting Joe in respiratory distress. He was no longer able to breathe entirely on his own. Subsequent tests throughout the day wouldn’t provide any insight and his condition was declining. It was recommended that Joe be transferred to another local hospital which has a designated Neurological Intensive Care Unit (ICU) and an ambulance was scheduled.
The ride in the ambulance that morning was terrifying. Almost immediately upon arrival at the Neurological ICU, the severity of everything became real and present. Joe was whisked away for further evaluation while the family was sent to wait outside. Still unsure of everything, we’d console each other as emotions became too overwhelming. We’d assure ourselves of a positive outcome but it was hard not to feel like we were all hovering just above despair. When we saw Joe next, he’d have multiple IV lines placed, his entire head was covered in electrodes and wires, and he’d been intubated with a nasotracheal tube to breathe for him. He was given sedatives to induce a comatose state and was on full life support.
Inducing a coma helped keep the tremors a bit calmer and within a few days of treatment, seizure activity had decreased dramatically. That first week was an endless stream of monitoring and testing, up to and including a spinal tap. The initial lab results and scans would rule out just about every common disease they could test for. His labs and cerebrospinal fluid were sent for more extensive testing. It would be over a month before these tests would yield some greater insight. Joe would continue to require sedation, daily tests would confirm this. During these tests, sedation was paused, allowing doctors to observe how patients react without it. Day after day, Joe would present the same; his entire body would go rigid and heavy tremors would resume leaving him stiff as a board, flailing uncontrollably. The sedation medications would restart and everyone would await the following day, hoping for a better result.
This is how the first month would continue to go. His autonomic dysfunction which affected his ANS was raging, pushing vitals into critical levels daily. This was all part of a process known as neurological storming. The storming also brought upon involuntary contractions called dystonia, which was accompanied with diaphoresis (heavy sweating). His nasotracheal tube was replaced with a full tracheostomy. A percutaneous endoscopic gastrostomy (PEG) tube was placed through the abdominal wall into the stomach providing a constant port for nutrition and medication. Immunotherapy treatments started days after arriving at the ICU. Early therapies included Intravenous Immunoglobulin (IVIG) and plasmapheresis (PLEX). Initial cycles wouldn’t provide any lasting relief so a new more aggressive cycle of therapy was devised. Another cycle of IVIG and PLEX would be administered but first, he’d receive four doses of Rituxan, one dose per week. Rituxan is a B-Cell depleting agent given to suppress the immune system. Aggressive treatment has shown benefits in autoimmune diseases and it was suspected what Joe was going through was autoimmune in nature. Joe had already been hospitalized for five weeks and was still unresponsive. We were being told it would be likely another month before they’d be able to ascertain any effects from this new treatment. It was also around this time that the lab work which was sent for more extensive testing had finally come in. A positive test showed elevated titers for an uncommon antibody, GAD-65. Based on his presentation and knowledge of this antibody, it allowed doctors to confirm what they had suspected. Joe was battling an extremely rare form of Encephalomyelitis known as Progressive Encephalomyelitis with Rigidity and Myoclonus (PERM).
The daily routine for that second month of hospitalization would continue similar to the first. With tremors occurring less frequently and less severe, his rigidity was used as a marker to gauge progress during the daily exams. Muscle relaxers and other medications used to treat these types of rigidity had not helped so any signs of less rigidness would likely be attributed to his overall neurological state improving. At its worst, there was zero flexibility. Any attempt to bend or maneuver limbs I’d describe as similar to attempting to bend a plane of glass with the uncertainty of if it might shatter! However, less severe tremor activity allowed more opportunity to try and interact with Joe while the sedation was being held. It was here, breaks in the clouds began to show, allowing rays of light to shine through. It took real effort to engage him as his eyes would need to be physically pried open. It was difficult to keep them open and even more difficult to get his attention. Still, something was happening. At first, it would only last a few seconds but looking at Joe and having him look back was such an incredible feeling for everyone! Although he doesn’t have any vivid memory of his hospitalization, on New Year’s Eve, Joe and I would watch as the ball dropped and they counted down the last ten seconds of 2017. During that moment, I felt very deeply that a new time had come.
It would be another six weeks before Joe would eventually be discharged from the ICU. The last month showed his condition not only stabilizing but improving. Episodes of storming became more predictable, therefore, treatable. Over that time, we even began to establish a reliable means of active communication! Yes or No questions would be answered occasionally with a slight nod or by using a communication board speech therapists use that could be placed in front of his hand so he could point a finger to the appropriate answer. Engagement was a game-changer. Not only were we able to get answers to the basic questions, Do you feel ok? Does this hurt? it was also evident that cognitively, he was fairing well. His recognition of events prior to getting sick was there; he knew who everyone was and he hadn’t lost much of his sarcasm. All these little indicators of progress during that time were immensely uplifting.
Longer periods of engagement also meant being able to assess what physical limitations had been imposed since the inception of all this. The first indicators were that essentially all basic motor coordination was significantly affected or lost entirely. Even the simple task of moving one finger a couple of inches left or right to point to ‘yes or no’ on his board took considerable effort and concentration. Bending limbs or any motion against gravity, such as lifting hands or legs off the bed, was unfeasible. When it came time for rehabilitation, Joe would now need to relearn just about everything he’d done his entire life. Intense rehabilitation doesn’t occur in a hospital bed and any chance of recovery would require just that. The longer it took to get medically stable enough to leave the hospital, the more muscle atrophy and weakness would occur. Tests done in late January would show that the most recent cycle of immunotherapies was having the desired effect and that helped validate the recent improvements we were seeing. Doctors felt more confident talking about devising a plan for the next step. The last big hurdle would be to wean Joe from the ventilator so he could move around unrestricted by a machine. Serious amounts of energy were allocated to this goal during the last month and another in what was becoming a huge series of hurdles was achieved. On February 14, 2018, after 99 days in ICU care, Joe would be leaving and the next step on his adventure was beginning.
It was the evening of the 14th when Joe arrived at a renowned Acute Rehabilitation Facility which was two and a half hours from home. This rehab facility has a specialty in treating neurological conditions. Their focus is to provide maximum healing during the acute phase of an illness or injury by providing aggressive rehabilitation. They also staff doctors and nurses onsite twenty-four hours for medical care. Here Joe would receive daily occupational, physical, and speech therapy sessions for a total of six hours a day and up to six days a week. In addition to the therapy sessions, Joe would no longer be confined to one room for the day. The facility provides community spaces for people to gather whenever they are not in therapy and this became a great outlet as Joe became more alert and frustrated with being constricted by his lack of independence.
When we arrived at the rehab facility, Joe still had his tracheal tube. He was no longer reliant on a ventilator to breathe for him but at times required supplemental oxygen when his O2 saturation would decrease. A collar could easily be placed over the tube to administer oxygen as needed but freed him up otherwise. This tube also provided an easy means to suction any secretions he could not clear, which was considered a safety net for when he would begin swallowing therapy. In the event of choking or aspiration, the obstruction or unwanted substance could be removed by way of suctioning it out through the tube. The tube that was placed in the ICU for ventilator use was larger than he would continue to need and also prevented him from talking. The pulmonologist suggested changing the current tube out for a smaller one and adding a speaker valve which would allow Joe to talk through it; if he was able. It had been over three months since he had used his voice! It’s not a difficult procedure so the doctor set it up and, within a few minutes, the tracheal tube was swapped out and sure enough, Joe was talking again! I do not remember what those exact first words were. There was a series of basic questions posed by the doctor to which he answered short one-word answers. The most vivid memory I have occurred the following day when his wife Danielle and our Mom came to visit. Danielle knew he was talking but Mom didn’t. As they came into the room and greeted Joe with the usual good mornings, I can recall the expression on Mom’s face as she looked at Joe in astonishment when he greeted her back! In typical Joe fashion, the first words Mom heard from him after all this time were, “You look like hell!” I’m certain she’d felt like she had gone, or was going through, a literal hell but that morning while Joe was in therapy, the family laughed and cried and we all embraced this surge of gratitude for where we’d come from and where we were.
It didn’t take long to adapt and appreciate the routine at the new facility and, aside from a lot of details, it started to resemble somewhat of a normal life. After the morning rounds of medications and tube feeding, staff would assist Joe with dressing into real clothes (no more hospital gowns!) and the therapy team would come to retrieve him. Initially, they would use a sling system attached to the ceiling, a Hoyer Lift, to raise Joe out of bed and place him into his wheelchair. A large portion of those early PT or OT sessions consisted of stretching and manual manipulation while strength and coordination needed to be built before he could move independently. Speech sessions were focused on cognitive rehabilitation and swallowing therapy. Cognitively, he was performing well so exercises and testing focused on this became mundane rather quickly but, stayed a small part of the regiment. Far more attention was paid to his swallowing deficits. The ultimate goal was to get him eating again but, as in everything relative to his recovery, nobody could provide any certainty. Every day, hundreds of times, Joe would be asked repeatedly to swallow his saliva. A lemon-flavored swab was used to stimulate saliva and reflexes. The risk of aspiration was too great for attempts at swallowing anything else and this routine became monotonous rather quickly. All therapy sessions were split into one hour per discipline in the morning and another hour in the afternoon. Much of the evening was free time. Free time felt like just that, freeing. Danielle and other families would visit multiple times a week. When it was just the two of us, we’d mosey about the floor chatting with other patients or staff. Joe could finally reimmerse himself in the world of sports, watching his teams play live and getting back into his online fantasy leagues. He loved that. Joe actually went into a coma halfway through his fantasy football season. There was nobody making changes or playing for him during that time and he still wound up winning his league! That’s Joe for ya! Once he began regaining some of his fine motor coordination in his fingers and hands, we’d spend a lot of time playing games. Especially his favorites, UNO and Yahtzee. My favorite times, and maybe his too, was when we’d venture outside to the courtyard where it was often cold and covered with snow in February. The sunshine and fresh air were too alluring after being confined for months so we’d bundle up and soak it all in, sometimes for hours.
Daily improvements were being seen early on. It was slow and incremental which is a trend that would continue throughout his entire recovery. Constant work was put into increasing mobility until Joe was beginning to move his limbs independently. He could hold and manipulate objects in his hand to some degree, and he could flex his legs all within the first couple of weeks. They’d begun to place in him a standing frame for extended periods of time allowing the body to adjust to being vertical. This would slowly build his strength by supporting his weight and holding him upright. His entire body was being reprogrammed, piece by piece, rebuilt with the eventual goal of getting everything to function as one cohesive unit. Each task had its own end goal. The goal of the standing frame was to get him comfortable enough to stay upright for when he was strong enough to attempt taking steps with a walker. Joe was also able to make headway with swallowing. The therapist was able to start introducing ice chips and Joe was doing well initiating a swallow. By the time his birthday came around in early March, they began doing some light food trials, and the finest Jello Pudding party I’d ever seen occurred!
Joe would ultimately spend just shy of two months in the acute rehabilitation facility. So many lessons were taken from our time here. By the end, Joe would meet the goal of walking 200 steps with a walker, unaided. He was able to complete many daily tasks unassisted from his wheelchair and so on. Pieces were finally coming back together. Above all the physical benefits, his energy levels were up. The daily grind of therapy and being engaged for so many hours of the day really helped to begin to lift Joe out of the lethargic state he was perpetually in when he got there. He was showing vigor towards his therapy and towards working to regain the life he knew. In early April 2018, as spring approached, our lives were full of new growth, meaning, and purpose. Five months had passed since the first seizure, and there were two little girls who’d been eagerly waiting for their Dad to come home. So, that’s where we headed!
Homelife was a bit different than what Joe remembered. A room was converted on the first floor to allow easier movement within the house. To some degree, it resembled the hospital rooms he’d stayed in. It had a hospital bed along with a dedicated closet for the medical equipment and supplies required for his care. The back door was outfitted with a wheelchair ramp for easier access in and out. Therapists would come to a couple of times a week for sessions. On the days when they wouldn’t, we would assist Joe in his exercises. Coming home did not signify a moment in which to slow down. Although he had made so much relative progress during his time at acute rehab, his deficits were still great. All the while, he was becoming more frustrated by the limitations that come with being unable to move unaided. The only way to continue to get better was to keep working and that’s what he did, every single day. No longer under the regiment of daily care and scheduled therapy sessions, we’d have to be creative at home. Every moment of the day would be analyzed to see if there were ways to use that time towards getting better. Rarely, did anything come free, and Joe would continue to push the limits of what his body could do on a daily basis. This would continue for around eighteen months.
On April 23, less than three weeks after leaving rehab, his tracheal tube would be removed. By June, the process of weaning him off of a list of medications spanning multiple pages had begun. The need for such a complex medication regimen was justified at first, but if they were no longer needed, it wouldn’t serve to keep administering the pills. The only way to find out was to try. Each medication was approached individually and weaned one at a time. Dosages would be tapered slowly over a week or two and a period of time was allocated to ascertain any effects of the removal. He was successful each time with every major neurological drug. Not only did this help confirm how much he was recovering, but he was also no longer dragged down by the side effects of the medications which often made him quite drowsy. By Christmas 2018, he would no longer require any neurological medications! His autonomic dysfunction stabilized, he was completely free of seizures and he was making the same level of physical gains without requiring muscle relaxers.
By July 2018, he was attending outpatient therapy with a more rigorous agenda than the home therapy team provided. He was now walking short distances using just a quad cane for balance. In September, he’d abandon the wheelchair for good only needing to use a single cane. Come late fall, he’d say goodbye to the cane, as well! On December 22nd, just in time for the holidays, he’d pass his final swallow test and was cleared for eating without restriction! This led to his PEG tube being removed from his stomach as he was consuming all nutrition by mouth. In early 2019, Joe was probably around 65% of his old self and becoming independent again. Therapy sessions at this point were geared towards strength training and increasing mobility. From the time we arrived at the acute rehab, a year prior, in February 2018, Joe’s personal motivation always reflected the big picture and achievement wouldn’t be recognized until he had made a full recovery. He was now left with only two major goals which, for him, would signify he had made his recovery. He’d made it out of the ICU alive, was independent in his own home, regularly visited with friends or family for shared meals and good times, and he attended all of his daughters’ school and sporting events. The last goals he held for himself were to return to the job he loved and to get back on a golf course. In January 2020, Joe returned to work full time for the same company he’d been with prior to his illness, a true testament of loyalty to them and also to Joe for his quality of work. Also, rest assured, Joe’s swinging a golf club as well as he ever has these days!
The individual physical achievements throughout would be far too great to list so instead, I encourage this. The next time you wake up, take a moment, and connect with your body. Fully immerse yourself in the minutiae of those first moments of your day and how your body moves. Consider all the parts. The muscles, tendons, ligaments, joints, and so on, that are required to get you to roll out of bed, stand up, balance yourself and start walking to where you want to go. What did it take to get that coffee cup out of the cabinet? How high did you have to reach? How many parts of your body really had to work collectively to achieve these simple mundane moments of your day? Joe came with a body that was locked stiff from the disease, nerves critically affected by neuropathy, and weakened severely from all the atrophy suffered after 90+ days immobile in the ICU.
If you didn’t know the story or had never met Joe in real life but were to meet him today, you’d never know that the man in front of you had beaten back death over and over to defy every odd and get to where he is. The fantastical recovery became Joe’s reality.
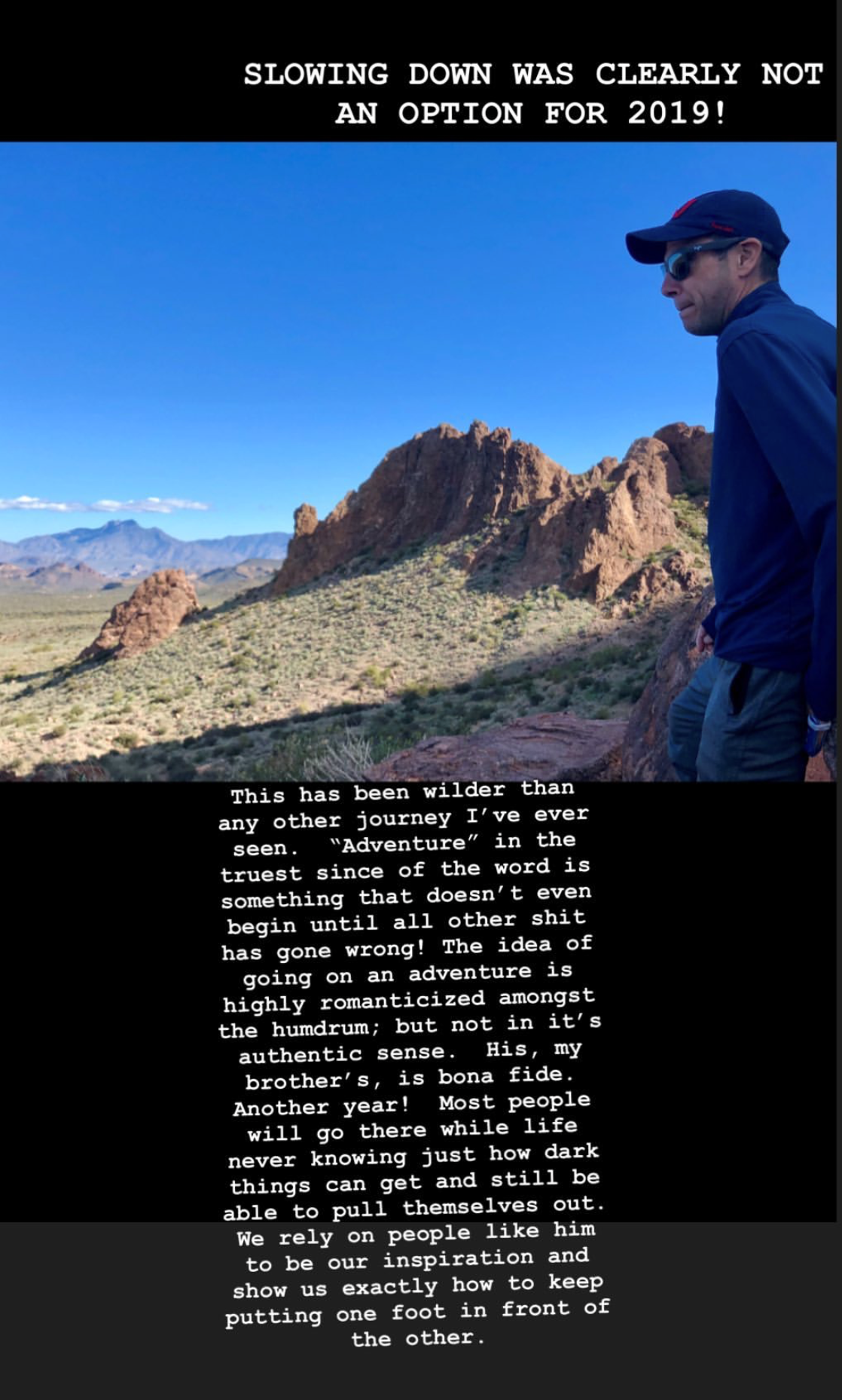
This has been wilder than any other journey I’ve ever seen. “Adventure,” in the truest sense of the word, is something that doesn’t begin until everything else has gone wrong. The idea of going on an adventure is highly romanticized amongst the humdrum; but not in its authentic sense. His, my brother’s, is bona fide.
Written by, Steve – Joe’s brother
Joe Calcagno, is our NYC support group leader, he is an amazing guy with a big heart, always there to support others.